Plaque Psoriasis
An individual with plaque psoriasis usually has patches of red, raised, scaly areas on the skin that may itch or burn. The patches are usually found on the knees, elbows, trunk, or scalp. Approximately 9 out of 10 people with psoriasis have plaque psoriasis.
The flare-ups can last for weeks or months. The psoriasis goes away for a time and then returns (chronic).
General characteristics of the scaly skin of the most common type of psoriasis are as follows:
Plaques: The plaque areas on the skin are elevated. The plaque areas vary in size (1 to several centimeters) and may range from a few to many at any given time on the skin. The shape of the plaque is usually oval but can be irregular in shape. Smaller plaque areas may merge with other areas and form a large affected area. The skin in these areas, especially when over joints or on the palms or feet, can split and bleed. Plaques sometimes have an area around them that looks like a halo or ring (Ring of Woronoff).

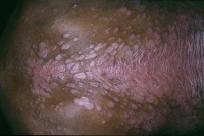
Plaque psoriasis with fissures, which are splits in the skin. Fissures usually occur where the skin bends (joints). The skin may bleed and is more susceptible to infection. Image courtesy of Hon Pak, MD.
Red color: The color of the affected skin is very distinctive. The rich, full red color is often called "salmon-colored." Sometimes the skin can have a blue tint when the psoriasis is on the legs.

Severe plaque psoriasis. Note the classic red color and scales or plaque. Image courtesy of Hon Pak, MD.
Scale: The scales are dry, thin, and silvery-white. The thickness of the scales may vary. When the scale is removed, the skin underneath looks smooth, red, and glossy. This shiny skin usually has small areas that bleed (Auspitz sign).
Plaque psoriasis. Image courtesy of Hon Pak, MD.
Symmetry: Psoriatic plaques tend to appear on both sides of the body in the same places. For example, the psoriasis is usually on both knees or both elbows at the same time.
Other general symptoms of plaque psoriasis are as follows:
Scalp: The scalp can have dry scaly skin or crusted plaque areas. Sometimes psoriasis of the scalp is confused with seborrheic dermatitis. In seborrheic psoriasis, the scales are greasy looking, not dry.

Psoriasis of the scalp. Image courtesy of Hon Pak, MD.
Nails: Nail changes are commonly observed in those with plaque psoriasis. The nails may have small indentations, ridges, or pits in them. The nails can be discolored or separate from the nail bed. (See Nail Psoriasis .)
Nail psoriasis. Note the classic pits and yellowish color in the nails. Image courtesy of Hon Pak, MD.
Psoriasis in children: Plaque psoriasis looks slightly different in children than in adults. In children, the plaques are not as thick and the affected skin is less scaly. Psoriasis may often appear in the diaper region in infancy and in flexural areas in children. The disease more commonly affects the face in children than in adults.
Other areas: Although the most common body areas affected are the arms, leg, back, and scalp, psoriasis can be found on any body part. Psoriasis can be found on the genitals or buttocks, under the breasts, or under the arms. These areas can feel especially itchy or burning.
Follow-up
Plaque psoriasis is a chronic disease that goes away and returns. Follow-up care depends on the severity of the disease at any given time.
If a patient has evidence of psoriatic arthritis, a consultation with a rheumatologist (one who specializes in
arthritis) is helpful.
Prevention
- Avoiding environmental factors that trigger psoriasis, such as
smoking, sun exposure, and s
stress, may help prevent or minimize flare-ups of psoriasis. Sun exposure may help in many cases of psoriasis and aggravate in others.
- Alcohol is considered a risk factor for psoriasis in young to middle-aged men. Avoid or minimize alcohol use if you have psoriasis.
- Specific dietary restrictions or supplements other than a well-balanced and adequate diet are unimportant in the management of plaque psoriasis.
Outlook
Psoriasis is more of an inconvenience in most cases than it is threatening. However, it is a chronic disease and reoccurs. The itching, peeling, splitting of skin at joints can lead to significant pain and self-esteem issues. By far, the patient's quality of life is affected most with plaque psoriasis. Self-consciousness and embarrassment about appearance, inconvenience, and high costs of treatment options all affect one's outlook when living with psoriasis.
Complications of the disease are relatively uncommon. Many of the complications of plaque psoriasis are related to the treatments used for the disease. Overly aggressive use of topical steroids could lead to more severe forms of psoriasis (from plaque to pustular for example). Topical steroids should not be used with bandages because inflammation and swelling may occur. Oversensitivity to the sun is possible with many of the treatment options (especially phototherapy).
About 10% percent of all cases of plaque psoriasis are associated with psoriatic arthritis.
Anxiety , depression , or stress may worsen symptoms and increase the tendency to itch.
Methotrexate, PUVA, cyclosporine, and oral retinoids all have helped to induce and maintain remission in severe cases of plaque psoriasis.
Top